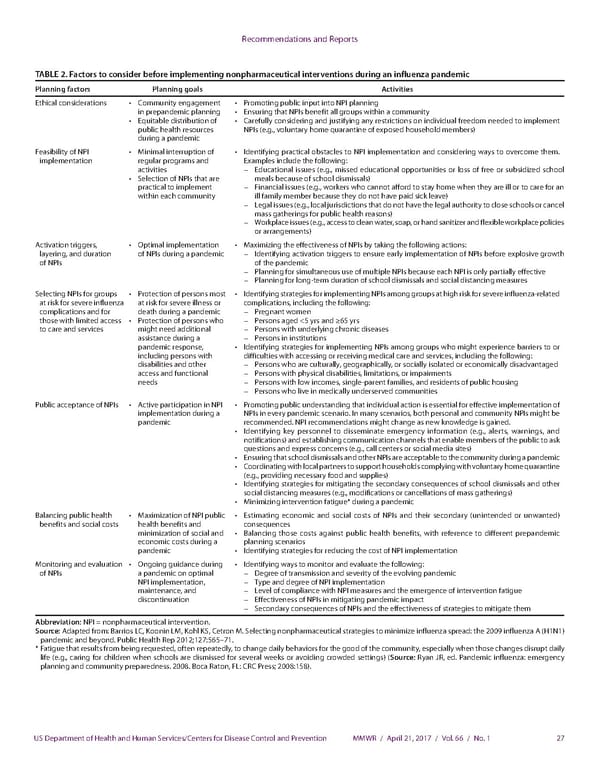
Recommendations and Reports TABLE 2. Factors to consider before implementing nonpharmaceutical interventions during an influenza pandemic Planning factors Planning goals Activities Ethical considerations • Community engagement • Promoting public input into NPI planning in prepandemic planning • Ensuring that NPIs benefit all groups within a community • Equitable distribution of • Carefully considering and justifying any restrictions on individual freedom needed to implement public health resources NPIs (e.g., voluntary home quarantine of exposed household members) during a pandemic Feasibility of NPI • Minimal interruption of • Identifying practical obstacles to NPI implementation and considering ways to overcome them. implementation regular programs and Examples include the following: activities – Educational issues (e.g., missed educational opportunities or loss of free or subsidized school • Selection of NPIs that are meals because of school dismissals) practical to implement – Financial issues (e.g., workers who cannot afford to stay home when they are ill or to care for an within each community ill family member because they do not have paid sick leave) – Legal issues (e.g., local jurisdictions that do not have the legal authority to close schools or cancel mass gatherings for public health reasons) – Workplace issues (e.g., access to clean water, soap, or hand sanitizer and flexible workplace policies or arrangements) Activation triggers, • Optimal implementation • Maximizing the effectiveness of NPIs by taking the following actions: layering, and duration of NPIs during a pandemic – Identifying activation triggers to ensure early implementation of NPIs before explosive growth of NPIs of the pandemic – Planning for simultaneous use of multiple NPIs because each NPI is only partially effective – Planning for long-term duration of school dismissals and social distancing measures Selecting NPIs for groups • Protection of persons most • Identifying strategies for implementing NPIs among groups at high risk for severe influenza-related at risk for severe influenza at risk for severe illness or complications, including the following: complications and for death during a pandemic – Pregnant women those with limited access • Protection of persons who – Persons aged <5 yrs and ≥65 yrs to care and services might need additional – Persons with underlying chronic diseases assistance during a – Persons in institutions pandemic response, • Identifying strategies for implementing NPIs among groups who might experience barriers to or including persons with difficulties with accessing or receiving medical care and services, including the following: disabilities and other – Persons who are culturally, geographically, or socially isolated or economically disadvantaged access and functional – Persons with physical disabilities, limitations, or impairments needs – Persons with low incomes, single-parent families, and residents of public housing – Persons who live in medically underserved communities Public acceptance of NPIs • Active participation in NPI • Promoting public understanding that individual action is essential for effective implementation of implementation during a NPIs in every pandemic scenario. In many scenarios, both personal and community NPIs might be pandemic recommended. NPI recommendations might change as new knowledge is gained. • Identifying key personnel to disseminate emergency information (e.g., alerts, warnings, and notifications) and establishing communication channels that enable members of the public to ask questions and express concerns (e.g., call centers or social media sites) • Ensuring that school dismissals and other NPIs are acceptable to the community during a pandemic • Coordinating with local partners to support households complying with voluntary home quarantine (e.g., providing necessary food and supplies) • Identifying strategies for mitigating the secondary consequences of school dismissals and other social distancing measures (e.g., modifications or cancellations of mass gatherings) • Minimizing intervention fatigue* during a pandemic Balancing public health • Maximization of NPI public • Estimating economic and social costs of NPIs and their secondary (unintended or unwanted) benefits and social costs health benefits and consequences minimization of social and • Balancing those costs against public health benefits, with reference to different prepandemic economic costs during a planning scenarios pandemic • Identifying strategies for reducing the cost of NPI implementation Monitoring and evaluation • Ongoing guidance during • Identifying ways to monitor and evaluate the following: of NPIs a pandemic on optimal – Degree of transmission and severity of the evolving pandemic NPI implementation, – Type and degree of NPI implementation maintenance, and – Level of compliance with NPI measures and the emergence of intervention fatigue discontinuation – Effectiveness of NPIs in mitigating pandemic impact – Secondary consequences of NPIs and the effectiveness of strategies to mitigate them Abbreviation: NPI = nonpharmaceutical intervention. Source: Adapted from: Barrios LC, Koonin LM, Kohl KS, Cetron M. Selecting nonpharmaceutical strategies to minimize influenza spread: the 2009 influenza A (H1N1) pandemic and beyond. Public Health Rep 2012;127:565–71. * Fatigue that results from being requested, often repeatedly, to change daily behaviors for the good of the community, especially when those changes disrupt daily life (e.g., caring for children when schools are dismissed for several weeks or avoiding crowded settings) (Source: Ryan JR, ed. Pandemic influenza: emergency planning and community preparedness. 2008. Boca Raton, FL: CRC Press; 2008:158). US Department of Health and Human Services/Centers for Disease Control and Prevention MMWR / April 21, 2017 / Vol. 66 / No. 1 27
 Community Mitigation Guidelines to Prevent Pandemic Influenza Page 28 Page 30
Community Mitigation Guidelines to Prevent Pandemic Influenza Page 28 Page 30